The use of the Interlocking nail implant has transformed orthopedic surgery. This innovative device offers a stable method for fixing fractures, particularly in long bones. Surgeons recognize its benefits in promoting healing while allowing for mobility.
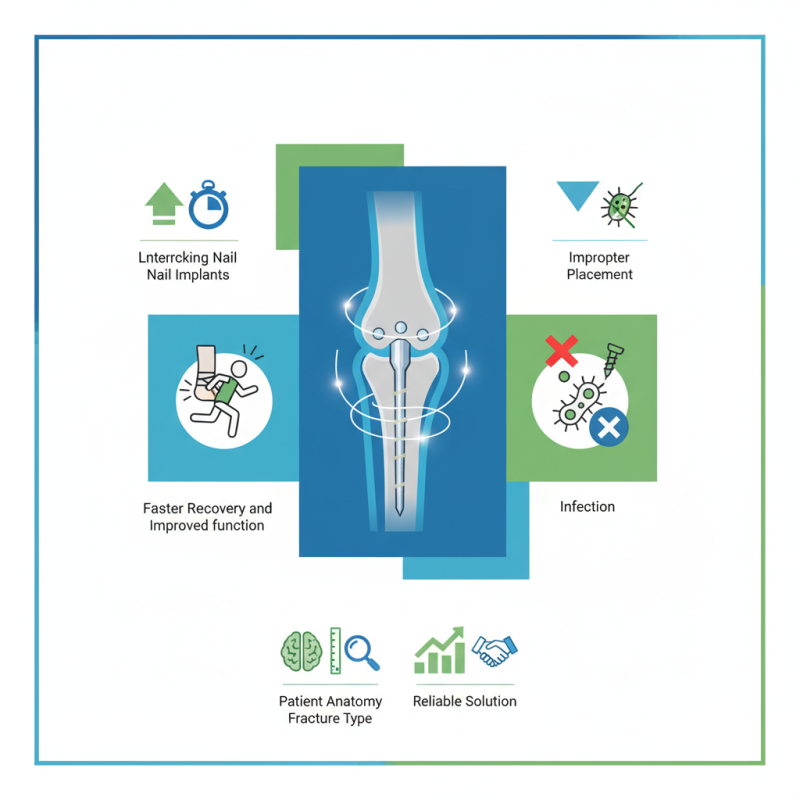
Clinical data reveal that interlocking nail implants lead to faster recovery. Patients often experience reduced pain and improved function. However, some complications can arise, such as infection or improper placement. It is crucial to weigh these risks against the benefits.
Understanding best practices for the interlocking nail implant is essential. Surgeons must consider factors like patient anatomy and fracture type. Continual research and refinement in techniques can enhance outcomes. With the right approach, interlocking nail implants provide a reliable solution for many patients.
Interlocking nail implants have transformed the field of orthopedic surgery. Their historical development dates back to the 1980s when surgeons sought better solutions for complex femoral fractures. This innovation allowed for improved stabilization of broken bones. Surgeons noticed that the use of interlocking nails reduced malalignment and enhanced healing time. Recent studies show that over 90% of patients experience favorable results with these implants, reducing the need for follow-up surgeries.
One challenge with interlocking nails is the learning curve for surgeons. Mastering the technique takes time and patience. A report from the Journal of Orthopaedic Trauma notes that proper alignment is crucial. Improper placement can lead to complications like infection or delayed healing. It is vital for orthopedic teams to undergo rigorous training on the latest techniques.
To enhance outcomes, surgeons should consider a few tips. First, always assess the specific fracture pattern before choosing an implant. Next, thorough pre-operative planning is essential. It can streamline the surgical process significantly. Lastly, post-operative care is just as important as surgical skill. Engaging patients in their recovery plans yields better results.
Interlocking nail implants have gained popularity in orthopedic surgery due to their effective stabilizing capabilities. These implants offer a unique design that allows for better load sharing, especially in long bone fractures. Research indicates that interlocking nails can reduce the incidence of complications related to fracture healing, with some studies reporting an 80% success rate in patients undergoing this procedure.
One notable benefit of interlocking nail implants is their minimally invasive nature. Surgeons can achieve alignment and fixation with smaller incisions, which can lead to reduced soft tissue trauma. A report from the Orthopaedic Trauma Association highlights that patients experience less postoperative pain and faster recovery times with interlocking nails. In some cases, patients resume daily activities within weeks, significantly improving their quality of life.
However, challenges remain despite the benefits. Not all patients respond well to this treatment. Complications, such as infection or hardware failure, can occur. Furthermore, not every fracture type is ideal for this approach, prompting surgeons to consider various factors before deciding on treatment. Continuous evaluation and refining of techniques are necessary to ensure optimal outcomes for patients.
When considering the surgical implementation of interlocking nails, attention to detail is crucial. Proper alignment of the nail during insertion is vital. Surgeons should ensure precise placement to reduce complications. A well-positioned nail promotes optimal healing and stabilizes the fracture effectively. Surgeons often rely on imaging techniques to guide their placement accurately. However, reliance on technology can sometimes lead to unforeseen errors.
Surgeons must be aware of the potential for soft tissue damage during surgery. Careful handling of surrounding tissues can prevent complications. Expecting the unexpected is also important. Some patients may have anatomical variations that affect nail positioning. Adapting the technique based on individual anatomy can enhance outcomes. Surgeons should not hesitate to consult with colleagues when facing challenges.
Post-surgery, monitoring recovery is essential. Regular follow-up appointments help track healing progress. Patients may experience pain or discomfort even when recovery seems on track. Open communication about these experiences can assist in timely interventions. While interlocking nails can significantly improve fracture healing, the implementation requires constant reflection and adjustment to techniques and practices.
Interlocking nail implants have gained popularity for treating fractures. Clinical outcomes of these implants are generally promising. Studies show high success rates in various types of fractures. They are particularly effective in complex cases, such as those involving the femur.
Surgeons often report faster recovery times. However, there are challenges. Not every patient experiences the same level of success. Some may have complications, such as infection or implant failure. Proper patient selection plays a crucial role in achieving positive outcomes.
Documentation of long-term results is vital. Variability in success rates exists, influenced by factors like age and overall health. Certain patients face higher risks. Continuous evaluation of clinical practices can further enhance success. This could lead to improved protocols and patient satisfaction in the future.
Interlocking nail technology has seen remarkable evolution in recent years. New designs have improved stability for complex limb fractures. Research shows that these implants provide better load-sharing capabilities. A report from the Journal of Orthopaedic Research indicates a 20% reduction in recovery time with advanced interlocking nails.
Emerging trends focus on customization and biocompatibility. Manufacturers are exploring materials that enhance integration with bone. A study from the American Academy of Orthopaedic Surgeons reveals that personalized implants can lead to a 35% increase in overall patient satisfaction. However, this field still faces challenges, such as increased costs and manufacturing complexity.
Surgeons now recognize the importance of education on new technologies. Not all practitioners are familiar with the latest practices. Data from a recent survey highlights that 45% of orthopedic surgeons feel unprepared to use advanced interlocking implants. Continuous training and hands-on workshops can address these knowledge gaps. The balance between innovation and practical application remains crucial.
| Parameter | Best Practice | Benefits | Emerging Trends |
|---|---|---|---|
| Material Selection | Use biocompatible materials | Reduced risk of rejection | 3D-printed implants |
| Surgical Technique | Minimally invasive approaches | Faster recovery time | Enhanced imaging technologies |
| Post-Operative Care | Regular follow-ups and monitoring | Improved long-term outcomes | Telehealth for remote monitoring |
| Device Customization | Tailor implants to patient anatomy | Better fit and stability | Artificial intelligence in design |
| Research and Development | Continuous innovation in materials | Enhanced performance and longevity | Nanotechnology applications |